How Bad are Your Headaches? Assessing Headache Burden
/When medical providers see a patient whose primary complaint is recurrent headache, it seems reasonable that one of the first questions asked would be: How bad are your headaches?
Unfortunately, if the headache disorder involved is migraine, the answer received may do little to assist in determining how much burden migraine is imposing upon the patient and, following from this, what specific treatment should be used to reduce that burden. It’s the rare patient who fails to respond, “My headaches are really bad, terrible, ruining my life, etc.” Makes sense; why would a person with headaches that are not especially bothersome go to the effort of making and keeping a medical appointment for headache evaluation?
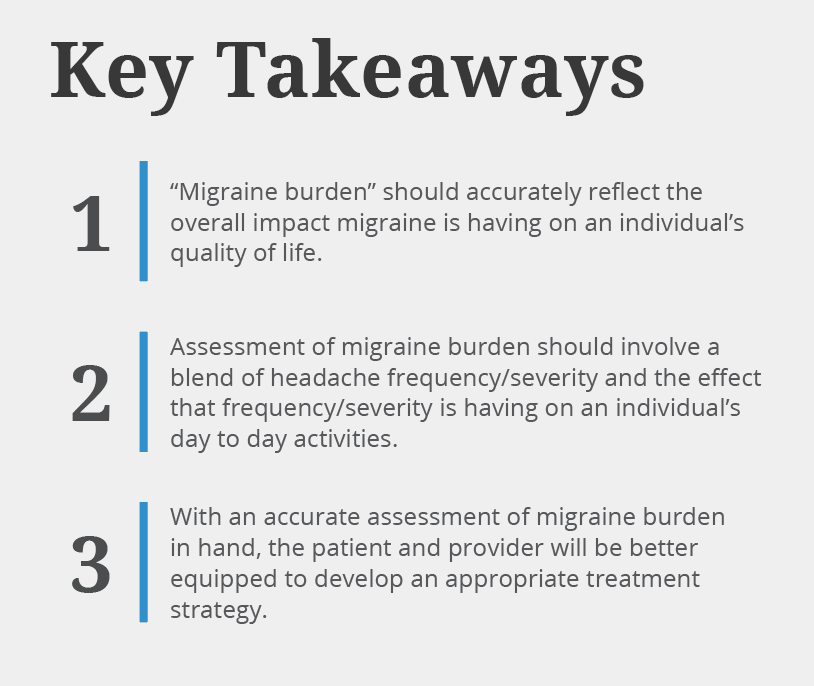
While any measure of “migraine burden” should include an assessment of headache frequency and severity, when you really think about migraine and the way it influences your quality of life, “migraine burden” is more than merely a function of how often you have a headache and how severe those headaches are. For example, how do you factor in the detrimental effects of migraine-associated nausea, vomiting, light sensitivity, sound sensitivity, sensitivity to odors, or sensitivity to motion? Or the distractions and concerns caused by migrainous aura? If you have vestibular migraine, it may be vertigo and disequilibrium that disrupt your life more than the headaches associated with migraine. How do you include this in calculating “burden”? What about the annoying effects of the prodromal and postdromal symptoms many migraineurs experience?
And what about the effect migraine has on your productivity at work and in other aspects of your life? Or the effect that it has on your relationship with others...your spouse/significant other, your children, your friends? Or simply your ability to enjoy your daily life? Do you love red wine, but avoid it because drinking a glass might precipitate a migraine attack? Are there other migraine “triggers” that you’ve eliminated from your life…to the detriment of your quality of life?
Do you suffer from “cephalalgiaphobia”, a tongue-twister of a word that literally means “fear of headache”? How often do you avoid or cancel an activity - a dinner date, a vacation, a family gathering - because of your fear that the activity may provoke an acute attack of migraine that ruins the activity for yourself and those around you? Aside from the time lost to episodes of acute headache, how else have you altered your life to accommodate migraine, this unwelcome companion? Ultimately, migraine burden represents the sum of a wide variety of factors that are negatively affecting your quality of life and the lives of those closest to you.
All of these factors contribute to the burden migraine imposes, and it is exceedingly difficult to come up with a number or another objective measure that can take them all into account. Over the years, clinical scientists involved in migraine research have developed increasingly sophisticated instruments that provide perspective on how migraine impacts the quality of life and how much, or little a given therapy is perceived by patients to improve their quality of life. Because of time constraints inherent in a busy clinic, however, few of those instruments have been transferred to routine clinical practice and the interaction between migraine patients and medical providers.
So how can you as a patient best convey to your provider a clear idea of your migraine burden? An article published in a previous issue of Migraineur provided a number of tips on how to prepare for your first visit to see a medical provider for evaluation of your migraine, and high on the list of those tips was keeping a headache diary. The ideal headache diary will provide the information most needed without overwhelming the provider with distracting and unnecessary details.
For a month or two, keep track of those days when you experience a headache of any severity which lasts for at least 4 hours or a headache of any duration for which you take medication (prescription or over-the-counter); include the name of any medication taken. In other words, how many “headache days” are you experiencing each month? Along with this, record how many of those days involve headache, which caused you to be unable to undertake your routine activities for at least one hour. In other words, how many “functionally incapacitating headache days” are you experiencing each month?
From this, you and your provider can calculate your “headache frequency/severity profile”. For example, if in the previous month you had 5 days of headache lasting 4 hours or more plus 3 additional days of shorter duration headache for which you took Excedrin (thus 8 “headache days” in total), and if 2 of those 8 days involved headache that prohibited routine daily activities for at least 1 hour (thus 2 “functionally incapacitating headache days”), then your frequency/severity profile was 8/2.
This information is critical to constructing an appropriate migraine treatment strategy. At the George Washington University Headache Center we use headache day frequency to divide our migraine patients into four groups: low frequency episodic (0-3 headache days/month), mid-frequency episodic (4-8 headache days/month), high frequency episodic (9-14 days/month) and chronic migraine (15 or more headache days/month). Whereas we rarely prescribe a prophylactic/prevention medication for patients with low-frequency episodic migraine, such medication almost invariably is prescribed for patients with high-frequency episodic migraine or chronic migraine. For patients with mid-frequency episodic migraine, the decision whether or not to begin prophylactic /prevention medication depends in part on the individual patient’s previous experience with acute/symptomatic medication and the severity of the headaches involved.
As mentioned previously, however, migraine burden is much more than a function of headache frequency and severity. While there are several instruments available which survey the effect migraine is having on your quality of life and which you may complete in advance of your appointment to give to your provider along with your frequency/severity profile, one of the most widely used and straightforward is the MIDAS (Migraine Disability Assessment) questionnaire. MIDAS provides a numerical assessment of migraine’s impact on your quality of life over the preceding 90 days, with questions related to work absenteeism, productivity at work or home, and migraine-related inability to participate in family, social or leisure activities.
Taken with the headache frequency/severity profile, your MIDAS score will assist you and your provider in making important decisions regarding a management strategy for your migraine.